| Dietary Approaches to Prevent and Treat Hypertension | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| A Scientific Statement from the American Heart Association Lawrence J. Appel, Michael W. Brands, Stephen R. Daniels, Njeri Karanja, Patricia J. Elmer, Frank M. Sacks. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A substantial body of evidence strongly supports the concept that multiple dietary factors affect blood pressure (BP). Well-established dietary modifications that lower BP are reduced salt intake, weight loss, and moderation of alcohol consumption (among those who drink). Over the past decade, increased potassium intake and consumption of dietary patterns based on the "DASH diet" have emerged as effective strategies that also lower BP. Of substantial public health relevance are findings related to blacks and older individuals. Specifically, blacks are especially sensitive to the BP-lowering effects of reduced salt intake, increased potassium intake, and the DASH diet. Furthermore, it is well documented that older individuals, a group at high risk for BP-related cardiovascular and renal diseases, can make and sustain dietary changes. The risk of cardiovascular disease increases progressively throughout the range of BP, beginning at 115/75 mm Hg. In view of the continuing epidemic of BP-related diseases and the increasing prevalence of hypertension, efforts to reduce BP in both nonhypertensive and hypertensive individuals are warranted. In nonhypertensive individuals, dietary changes can lower BP and prevent hypertension. In uncomplicated stage I hypertension (systolic BP of 140 to 159 mm Hg or diastolic BP of 90 to 99 mm Hg), dietary changes serve as initial treatment before drug therapy. In those hypertensive patients already on drug therapy, lifestyle modifications, particularly a reduced salt intake, can further lower BP. The current challenge to healthcare providers, researchers, government officials, and the general public is developing and implementing effective clinical and public health strategies that lead to sustained dietary changes among individuals and more broadly among whole populations. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
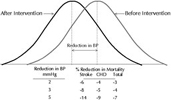
Elevated blood pressure (BP) remains an extraordinarily common and important risk factor for cardiovascular and renal diseases, including stroke, coronary heart disease, heart failure, and kidney failure. According to the most recent NHANES survey (1999 to 2000), 27% of adult Americans have hypertension (systolic BP 140 mm Hg, diastolic BP 90 mm Hg, or use of antihypertensive medication), and another 31% have prehypertension (systolic BP of 120 to 139 mm Hg or diastolic BP of 80 to 89 mm Hg, not on medication).1 Prehypertensive individuals have a high probability of developing hypertension and carry an excess risk of cardiovascular disease as compared with those with a normal BP (systolic BP <120 mm Hg and diastolic BP <80 mm Hg).2 It has been estimated that among adults >50 years of age, the lifetime risk of developing hypertension approaches 90%.3 Recent data indicate that the prevalence of hypertension is increasing4 and that control rates among those with hypertension remain low.5 On average, blacks have higher BP than nonblacks,4 as well as an increased risk of BP-related complications, particularly stroke6,7 and kidney failure.8 Elevated BP results from environmental factors, genetic factors, and interactions among these factors. Of the environmental factors that affect BP (diet, physical inactivity, toxins, and psychosocial factors), dietary factors have a prominent, and likely predominant, role in BP homeostasis. In nonhypertensive individuals, including those with prehypertension, dietary changes that lower BP have the potential to prevent hypertension and more broadly to reduce BP and thereby lower the risk of BP-related clinical complications. Indeed, even an apparently small reduction in BP, if applied to an entire population, could have an enormous beneficial impact. For instance, it has been estimated that a 3–mm Hg reduction in systolic BP could lead to an 8% reduction in stroke mortality and a 5% reduction in mortality from coronary heart disease (see Figure 1).12 In uncomplicated stage I hypertension (systolic BP of 140 to 159 mm Hg or diastolic BP of 90 to 99 mm Hg), dietary changes can serve as initial treatment before the start of drug therapy. Among hypertensive individuals who are already on drug therapy, dietary changes, particularly a reduced salt intake, can further lower BP and facilitate medication step-down. In general, the extent of BP reduction from dietary therapies is greater in hypertensive than in nonhypertensive individuals. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The purpose of this scientific statement, which updates prior AHA recommendations,13 is to summarize evidence on the efficacy of diet-related factors that lower BP and to present recommendations for healthcare providers, policy makers, and the general public. This document relies primarily on evidence as compiled in systematic reviews. Individual studies that document seminal findings are also discussed. Recommendations in this document are broadly consistent with those expressed in federal policy documents.9, 1. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Weight Loss
A substantial and largely consistent body of evidence from observational studies and clinical trials documents that weight is directly associated with BP. The importance of this relationship is reinforced by the high and increasing prevalence of overweight and obesity in the United States and throughout the world. Approximately 65% of US adults have a body mass index (BMI) 25 kg/m2 and therefore are classified as either overweight or obese; >30% of US adults are clinically obese (BMI 30 kg/m2).15 In US children and adolescents, the prevalence of overweight has increased over the past decade, as have levels of BP.16 With rare exception, clinical trials have documented that weight loss lowers BP. Importantly, reductions in BP occur before, and without, attainment of a desirable body weight. In one meta-analysis that aggregated results across 25 trials, mean systolic and diastolic BP reductions from an average weight loss of 5.1 kg were 4.4 and 3.6 mm Hg, respectively.17 In subgroup analyses, BP reductions were similar for nonhypertensive and hypertensive subjects but were greater in those who lost more weight. Within-trial dose–response analyses18, 19 and prospective observational studies20 also document that greater weight loss leads to greater BP reduction. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Table 1. Diet-Related Lifestyle Modifications That Effectively Lower BP | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Additional trials have documented that modest weight loss, with or without sodium reduction, can prevent hypertension by 20% among overweight, prehypertensive individuals21 and can facilitate medication step-down and drug withdrawal.22, 23 Lifestyle intervention trials have uniformly achieved short-term weight loss, primarily through a reduction in total caloric intake. In several instances, substantial weight loss has been sustained over 3 years.23, 24 Maintaining a high level of physical activity is well recognized as a critical factor in sustaining weight loss. Whether weight loss can blunt the age-related rise in BP is unclear. In one trial with long-term follow-up, those individuals who sustained a >10-lb weight loss achieved a lower BP that nonetheless rose over time.19 In aggregate, available evidence strongly supports weight reduction, ideally attainment of a BMI <25 kg/m2, as an effective approach to prevent and treat hypertension. More importantly, in view of the well-recognized difficulties of sustaining weight loss, efforts to prevent weight gain among those who have normal body weight are critically important. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
On average, as dietary salt (sodium chloride) intake rises, so does BP. Evidence includes results from animal studies, epidemiological studies, clinical trials, and meta-analyses of trials. To date, >50 randomized trials have been conducted. In one of the most recent meta-analyses,25 a median reduction in urinary sodium of 1.8 g/d (78 mmol/d) lowered systolic BP and diastolic BP by 2.0 and 1.0 mm Hg in nonhypertensive and by 5.0 and 2.7 mm Hg in hypertensive individuals. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In addition to reduced BP, clinical trials have documented that a reduced sodium intake can prevent hypertension (relative risk reduction of 20% with or without concomitant weight loss),21 can lower BP in the setting of antihypertensive medication,31, 32 and can facilitate hypertension control.22, 23 In observational studies, reduced sodium intake is associated with a blunted age-related rise in systolic BP.33 In other observational studies, reduced salt intake is associated with a reduced risk of atherosclerotic cardiovascular events34, 35 and congestive heart failure.36 The BP response to changes in dietary sodium intake is heterogeneous37 (as is the BP response to other dietary changes). Despite use of the terms "salt sensitive" and "salt resistant" to classify individuals in research studies, the change in BP in response to a change in salt intake is not binary.38 Rather, the reduction in BP from a reduced sodium intake has a continuous distribution, with individuals having greater or lesser degrees of BP reduction. In general, the effects of sodium reduction on BP tend to be greater in blacks; middle-aged and older persons; and individuals with hypertension, diabetes, or chronic kidney disease. These groups tend to have a less responsive renin-angiotensin-aldosterone system.39 It has been hypothesized that salt sensitivity is a phenotype that reflects subclinical renal disease.40 As discussed later in this statement, genetic and dietary factors also influence the response to sodium reduction. For example, the rise in BP for a given increase in sodium intake is blunted in the setting of either the DASH diet28 or high potassium intake.41, 42 Some salt intake is required. Recently, an Institute of Medicine committee set 1.5 g/d (65 mmol/d) sodium as an adequate intake level, primarily to ensure nutrient adequacy.43 Although a sodium intake below this level is associated with lower BP,44 little information is available about the nutrient content of diets that provide <1.5 g/d of sodium. From the DASH-Sodium trial, it is apparent that Western-type diets can provide this level of sodium intake and that such a diet can also provide adequate levels of other nutrients.45 Because the relationship between sodium intake and BP is direct and progressive without an apparent threshold, it is difficult to set an upper level of sodium intake, which also could be 1.5 g/d (65 mmol/d). However, in view of the available food supply and the currently high levels of sodium consumption, a reduction in sodium intake to 1.5 g/d (65 mmol/d) is not easily achievable at present. In the interim, a reasonable recommendation is an upper limit of 2.3 g/d (100 mmol/d), which is similar to earlier recommendations for the prevention and treatment of hypertension.9, 14 In aggregate, available data strongly support current, population-wide recommendations to lower salt intake. To reduce salt intake, consumers should choose foods low in salt and limit the amount of salt added to food. However, because >75% of consumed salt comes from processed foods,46 any meaningful strategy to reduce salt intake must involve the efforts of food manufacturers and restaurants, which should progressively reduce the salt added to foods by 50% over the next 10 years.9, 47 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
High potassium intake is associated with reduced BP. Evidence includes animal studies, observational epidemiological studies, >30 clinical trials, and meta-analyses of these trials. Although data from individual trials have been inconsistent, 3 meta-analyses of these trials have documented a significant inverse relationship between potassium intake and BP in nonhypertensive and hypertensive individuals.48–50 In the meta-analysis by Whelton et al,49 average systolic and diastolic BP reductions associated with a net increase in urinary potassium excretion of 2 g/d (50 mmol/d) were 4.4 and 2.5 mm Hg in hypertensive and 1.8 and 1.0 mm Hg in nonhypertensive individuals. Because no trial has tested the effects of 3 levels of dietary potassium intake on BP, inferences on the dose–response relationship between potassium and BP must be drawn from individual trials. Available data suggest that increased potassium has beneficial effects on BP in the setting of a low intake (eg, 1.3 to 1.4 g/d, or 35 to 40 mmol/d)51 or a much higher intake (eg, 3.3 g/d, or 84 mmol/d).52 Potassium reduces BP to a greater extent in blacks than in whites.49 In several trials, the effects of increased potassium intake in blacks have been particularly striking.53 Because a high potassium intake can be achieved through diet rather than pills and because potassium derived from foods is also accompanied by a variety of other nutrients, the preferred strategy to increase potassium intake is to consume foods such as fruits and vegetables that are rich in potassium, rather than supplements. In the DASH trial, the 2 groups that increased fruit and vegetable consumption both lowered BP.28, 54 The 2100-kcal version of the DASH diet provides 4.7 g/d (120 mmol/d) potassium.55 Another trial documented that increased fruit and vegetable consumption lowers BP, but it did not specify the amount of potassium provided in the fruits and vegetables.56 The effects of potassium on BP depend on the concurrent intake of salt and vice versa. Specifically, an increased intake of potassium has a greater BP-lowering effect in the context of a higher salt intake and lesser BP reduction in the setting of a lower salt intake. Conversely, the BP reduction from a reduced salt intake is greatest when potassium intake is low. For example, a high potassium intake (120 mmol/d) blunted the rise in BP in response to increased salt intake in 24 nonhypertensive black men and to a lesser extent in 14 nonblacks.42 In a 2x2 factorial trial that tested the effects of reduced salt intake and increased potassium intake, alone or together, on BP in 212 hypertensives,57 a reduced sodium intake lowered BP to the same extent as an increased potassium intake; however, the combination of both sodium reduction and increased potassium did not further lower BP. These data are consistent with subadditive effects of reduced salt intake and increased potassium intake on BP. The dearth of dose–response trials precludes a firm recommendation for a specific level of potassium intake as a means to lower BP. However, it is reasonable to set the recommended potassium intake level as 4.7 g/d (120 mmol/d). This level of intake corresponds to the average total potassium intake in clinical trials,49 the highest dose in the one available dose–response trial,42 and the potassium content of the DASH diet intake.54 It is also the adequate intake level set by an Institute of Medicine committee.43 On the basis of data from NHANES III, the average intake of potassium is 2.9 to 3.2 mg/d (74 to 82 mmol/d) in adult men and 2.1 to 2.3 g/d (54 to 59 mmol/d) in adult women; only 10% of men and <1% of women are consuming 4.7 g/d (120 mmol/d) potassium.43 In the generally healthy population with normal kidney function, a potassium intake from foods >4.7 g/d (120 mmol/d) poses no risk because excess potassium is readily excreted in the urine. However, in individuals whose urinary potassium excretion is impaired, a potassium intake <4.7 g/d (120 mmol/d) is appropriate because of adverse cardiac effects (arrhythmias) from hyperkalemia. Common drugs that can substantially impair potassium excretion are ACE inhibitors, angiotensin receptor blockers, nonsteroidal antiinflammatory agents, and potassium-sparing diuretics. Medical conditions associated with impaired potassium excretion include diabetes, chronic renal insufficiency, end-stage renal disease, severe heart failure, and adrenal insufficiency. Elderly individuals are at increased risk of hyperkalemia because they often have one or more of these conditions or take one or more medications that impair potassium excretion. The available evidence is insufficient to identify the level of kidney function at which individuals with chronic kidney disease are at increased risk for hyperkalemia from high potassium intake. However, an expert panel recommended that individuals with stage 3 or 4 chronic kidney disease, ie, an estimated glomerular filtration rate <60 mL · min–1 · 1.73 m–2, restrict their intake of potassium.58 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Observational studies and clinical trials have documented a direct, dose-dependent relationship between alcohol intake and BP, particularly as the intake of alcohol increases above 2 drinks per day.59, 60 Importantly, this relationship has been shown to be independent of potential confounders such as age, obesity, and salt intake.61 Although some studies have shown that the alcohol–hypertension relationship also extends into the light drinking range (2 drinks per day), this is the range in which alcohol may reduce coronary heart disease risk. A recent meta-analysis of 15 randomized controlled trials60 reported that decreased consumption of alcohol (median reduction in self-reported alcohol consumption, 76%; range, 16% to 100%) reduced systolic and diastolic BPs by 3.3 and 2.0 mm Hg, respectively. BP reductions were similar in nonhypertensive and hypertensive individuals. Importantly, the relationship between reduction in mean percentage of alcohol and decline in BP was dose dependent. In aggregate, available evidence supports moderation of alcohol intake (among those who drink) as an effective approach to lower BP. Alcohol consumption should be limited to 2 alcoholic drinks per day in most men and 1 alcoholic drink per day in women and lighter-weight persons. Note that 1 drink is defined as 12 oz of regular beer, 5 oz of wine (12% alcohol), and 1.5 oz of 80-proof distilled spirits. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
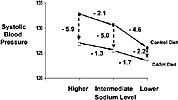
Vegetarian Diets Vegetarian diets have been associated with low BP. In industrialized countries, where elevated BP is commonplace, individuals who consume a vegetarian diet have markedly lower BPs than do nonvegetarians.62, 63 In these observational studies, vegetarians also experience a lower age-related rise in BP. Some of the lowest BPs observed in industrialized countries have been documented in strict vegetarians (macrobiotics) living in Massachusetts.64 Several aspects of a vegetarian lifestyle might lower BP, including nondietary factors (eg, physical activity), established dietary risk factors (eg, reduced weight, increased potassium, and low-to-moderate alcohol intake), and other aspects of vegetarian diets (eg, high fiber, no meat). To a variable extent, observational studies have controlled for the well-established determinants of BP. For instance, in a study of Seventh Day Adventists, analyses were adjusted for weight but not dietary sodium or potassium.63 Trial evidence, albeit limited, indicates that nondietary factors and established dietary risk factors are not fully responsible for the BP-lowering effects of vegetarian diets and that some other aspects of vegetarian diets lower BP. In the 2 available trials, one in nonhypertensive individuals65 and another in hypertensive persons,66 lactoovovegetarian diets reduced systolic BP by 5 mm Hg but had equivocal effects on diastolic BP. The DASH Diet and Related Dietary Patterns series of 3 large, controlled feeding studies tested the effects of dietary patterns on BP.28, 54, 67 The first trial was a randomized feeding study that compared 3 dietary patterns.54 Of the 3 diets studied, the most effective diet, now called the DASH diet, emphasized fruits, vegetables, and low-fat dairy products; included whole grains, poultry, fish and nuts; and was reduced in fats, red meat, sweets, and sugar-containing beverages. Accordingly, it was rich in potassium, magnesium, calcium, and fiber and was reduced in total fat, saturated fat, and cholesterol; it also was slightly increased in protein.55 It is likely that several aspects of the diet, rather than just one nutrient or food, reduced BP. Among all participants, the DASH diet significantly lowered mean systolic BP by 5.5 mm Hg and mean diastolic BP by 3.0 mm Hg, each net of changes in the control diet. A second diet, which emphasized just fruits and vegetables, also significantly reduced BP but to a lesser extent, about half of the effect of the DASH diet. The effects of the diets were rapid, occurring within only 2 weeks (see Figure 3). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The OmniHeart trial compared the effects of 3 healthy dietary patterns: a diet rich in carbohydrate (58% of total calories), a second diet rich in protein (about half from plant sources), and a third diet rich in unsaturated fat (predominantly monounsaturated fat).67 Similar to the DASH diet, each of the OmniHeart diets was reduced in saturated fat and cholesterol and rich in fruit, vegetables, fiber, potassium, and other minerals at recommended levels. As displayed in Figure 4, each diet lowered systolic BP. Furthermore, substituting some of the carbohydrate (10% of total kcal) with either protein (about half from plant sources) or unsaturated fat (mostly monounsaturated fat) further lowered BP. The DASH diet and the diets studied in the OmniHeart trial are safe and broadly applicable to the general population. However, because of their relatively high potassium and phosphorus content (in all diets) and high protein content (in the DASH diet and the protein-rich diet in OmniHeart), these diets are not recommended in persons with stage 3 or 4 chronic kidney disease, ie, an estimated glomerular filtration rate <60 mL · min–1 · 1.73 m–2.58. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Fish Oil Supplementation Several predominantly small clinical trials and meta-analyses of these trials69–71 have documented that high-dose omega-3 polyunsaturated fatty acid (commonly called fish oil) supplements can lower BP in hypertensive individuals. In nonhypertensive individuals, BP reductions tend to be small or nonsignificant. The effect of fish oil appears to be dose dependent, with BP reductions occurring at relatively high doses—namely, 3 g/d. In hypertensive individuals, average systolic and diastolic BP reductions were 4.0 and 2.5 mm Hg, respectively.71 Side effects, including belching and a fishy taste, are commonplace. In view of the high dose required to lower BP and the side-effect profile, fish oil supplements cannot be routinely recommended as a means to lower BP. Fiber Dietary fiber consists of the indigestible components of food from plants. Evidence from observational studies and several clinical trials suggests that increased fiber intake may reduce BP.72 More than 40 randomized trials of dietary fiber supplementation have been conducted. Still, most did not have BP as their primary outcome, and many had a multicomponent intervention. A meta-analysis of these trials,73 restricted to the 20 trials that increased just fiber intake, documented that supplemental fiber (average increase, 14 g/d) was associated with net systolic and diastolic BP reductions of 1.6 and 2.0 mm Hg, respectively. Subsequently, in a large randomized trial,74 supplemental fiber did not lower BP. Overall, data are insufficient to recommend an increased intake of fiber alone as a means to lower BP. Calcium and Magnesium Evidence that calcium intake might affect BP comes from a variety of sources, including animal studies, observational studies, clinical trials, and meta-analyses. In a meta-analysis of 23 observational studies, Cappuccio et al75 reported an inverse association between BP and dietary calcium intake (as measured by 24-hour dietary recalls or food frequency questionnaires). However, the size of the effect was relatively small, and there was evidence of publication bias and of heterogeneity across studies. Subsequently, meta-analyses of clinical trials documented modest reductions in systolic and diastolic BPs of 0.9 to 1.4 mm Hg and 0.2 to 0.8 mm Hg, respectively, with calcium supplementation (400 to 2000 mg/d).76–78 Also, some evidence indicates that the level of calcium intake may affect the BP response to salt. In 3 small trials, calcium supplementation attenuated the effect of a high sodium intake on BP.79–81 The body of evidence implicating magnesium as a major determinant of BP is inconsistent. In observational studies, often cross-sectional in design, a common finding is an inverse association of dietary magnesium with BP. In a pooled analysis of 29 observational studies, there was a negative association between dietary magnesium and BP.82 However, in a meta-analysis of 20 randomized clinical trials, no clear effect of magnesium intake on BP was evident.83 Overall, data are insufficient to recommend either supplemental calcium or magnesium as a means to lower BP. Carbohydrate An evolving but complex body of evidence suggests that both amount and type of carbohydrate intake affect BP.84 Worldwide, there are many populations that eat carbohydrate-rich, low-fat diets that have low BP levels as compared with Western countries.62 Still, the results of observational studies that specifically examined the effect of carbohydrate intake on BP have been inconsistent (direct in one study,85 no association in another,86 and inverse association in another87). In early, albeit small, trials, increasing carbohydrate by reducing total fat generally did not reduce BP.88 In contrast, the recently completed OmniHeart feeding study documented that in the setting of a healthy diet similar to the DASH diet, partial substitution of carbohydrate with either protein (about half from plant sources) or monounsaturated fat lowers BP; importantly, the total dietary glycemic index, an indicator of the type of carbohydrate, was moderate and similar in each diet.67 Note that the incremental effects on BP of replacing some carbohydrate with protein or monounsaturated fat were modest as compared with the large effects of the carbohydrate-rich diet studied in the OmniHeart study (see Figure 4)67 or the DASH diet itself (Figure 3).54 A few trials have also tested the effects of short-term sugar consumption on BP. In several89, 90 but not all studies,91 consumption of sugars raised BP. Consistent with these studies are results from a weight loss trial in which a low–glycemic-index diet reduced BP to a greater extent than a standard high–glycemic-index diet.92 Overall, additional research is warranted before specific recommendations can be made about the amount and type of carbohydrate. Intake of Fats Other than n-3 PUFA Total fat includes saturated fat, omega-3 polyunsaturated fat, omega-6 polyunsaturated fat, and monounsaturated fat. Although early studies focused on the effects of total fat intake on BP, there is a plausible biological basis to hypothesize that certain types of fat (eg, omega-3 polyunsaturated fat) might reduce BP and that other types of fat (eg, saturated fat) might raise BP. Hence, the direction of the BP effect might be direct (positive) or inverse, depending on the type of fats consumed. Saturated Fat Several observational studies and a few clinical trials have assessed the impact of saturated fat on BP. In the vast majority of studies, including 2 prospective observational studies, the Nurses Health Study and the Health Professional Follow-up Study, saturated fat intake (percent kilocalories as determined by a food frequency questionnaire) was not associated with incident hypertension.93, 94 In the few available trials, diet interventions that focused only on reducing saturated fat had no significant effect on BP.88 Because most trials tested diets that were both reduced in saturated fat and increased in polyunsaturated fat, the absence of an effect on BP also suggests no benefit from polyunsaturated fat. Omega-6 Polyunsaturated Fat Intake Dietary intake of omega-6 polyunsaturated fat (mainly linoleic acid in Western diets) has little effect on BP. In an overview of cross-sectional studies that correlated BP with tissue or blood levels of omega-6 polyunsaturated fat, there was no apparent relationship (no association in 8 studies, inverse association in 4 studies, and 1 positive association).88 Prospective observational studies and clinical trials have likewise been unsupportive of a relationship.88, 93, 94 Monounsaturated Fat Intake Few studies have assessed the relationship between monounsaturated fat intake and BP. Five of 7 cross-sectional studies did not detect a relationship,88 and neither of 2 prospective studies conducted in the United States documented an effect of monounsaturated fat intake on subsequent hypertension.93, 94 Likewise, evidence from the earliest clinical trials did not support a relationship between monounsaturated fat and BP.88 However, subsequent trials have shown that diets rich in monounsaturated fats lower BP.95, 96 In the recently completed OmniHeart study, partial substitution of carbohydrate with monounsaturated fat lowered BP. Overall, although increased monounsaturated fat appears to lower BP, this relationship often is confounded by a concomitant reduction in carbohydrate intake. Hence, the effect of monounsaturated fat intake per se on BP is uncertain.67 Protein Intake An extensive, and generally consistent, body of evidence from observational studies has documented significant inverse associations between protein intake and BP.73, 97 Recently, 2 major observational studies, the International Study on Macronutrients and Blood Pressure (INTERMAP) and the Chicago Western Electric Study, have documented significant inverse relationships between protein intake and BP.87, 98 In these studies, protein from plant sources was associated with lower BP, whereas protein from animal sources had no effect. Some trials have also examined the effects of increased protein intake on BP. Most of these trials tested soy-based interventions on BP. In some but not all of these trials, soy supplementation replacing carbohydrate reduced BP.99, 100 In a recent large trial conducted in China, replacing carbohydrate with increased protein intake from soy supplements lowered BP.101 In the recently completed OmniHeart study, partial substitution of carbohydrate with protein (about half from plant sources) lowered BP.67 In aggregate, data from clinical trials, in conjunction with evidence from observational studies, support the hypothesis that substitution of carbohydrate with increased intake of protein, particularly from plants, can lower BP. However, it remains uncertain whether the effects result from increased protein or reduced carbohydrate. Cholesterol Few studies have examined the effect of dietary cholesterol intake on BP. In the Multiple Risk Factor Intervention Trial (MRFIT) cohort, there were significant, direct relationships between cholesterol intake (in milligrams per day) and both systolic and diastolic BPs.85 The Keys score was also associated with diastolic but not systolic BP. In longitudinal multivariate analyses from the Western Electric Study, there were significant positive relationships of change in systolic BP over 8 years with both dietary cholesterol and Keys score.87 Still, despite these consistent reports from 2 studies, the paucity of evidence precludes any conclusion about a relationship between dietary cholesterol intake and BP. Vitamin C Laboratory studies, depletion–repletion studies, and epidemiological studies suggest that increased vitamin C intake or status is associated with lower BP. In a systematic review by Ness et al,102 10 of 14 cross-sectional studies reported an inverse association between plasma vitamin C and BP, and 3 of 4 reported an inverse association with vitamin C intake. The 2 nonrandomized and 4 randomized controlled trials were all small, and results were inconsistent; effect sizes ranged from 0 to >10 mm Hg in systolic BP reduction. In a subsequent trial, 500 mg of vitamin C had no effect on BP over the course of 5 years.103 In summary, it remains unclear whether an increased intake of vitamin C reduces BP. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A rapidly increasing body of evidence indicates that genetic factors affect BP levels and the BP response to dietary changes. Most of the available evidence has focused on genetic factors that influence the BP response to salt intake. Several genotypes that influence BP have been identified. Most of these genotypes influence the renin-angiotensin-aldosterone axis or renal salt handling. In a line of investigation that focused on mendelian diseases associated with either high or low BP, 6 genes associated with higher BP and another 8 genes associated with lower BP have been identified.104 It is noteworthy that each of these genes regulates renal sodium chloride handling; mutations that increase net sodium chloride reabsorption raise BP, whereas mutations that reduce sodium chloride reabsorption lower BP. Table 2: Effects of Dietary Factors and Dietary Patterns on BP: A Summary of the Evidence |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Several trials have examined the effects of specific genotypes on the BP response to dietary changes. In 3 trials, genetic variation of the angiotensinogen gene modified the BP response to changes in salt intake in nonblacks26, 105, 106 and the BP responses to weight loss105 and the DASH diet.107 Polymorphism of the -adducin gene also appears to affect the BP response to salt.108 Finally, the ACE insertion-deletion polymorphism may affect the BP response to weight loss.109 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Despite the potential for substantial reductions in BP from simultaneous implementation of multiple lifestyle interventions, few trials have examined the combined impact of multicomponent interventions. In general, multicomponent intervention studies have documented subadditivity; ie, the combined effect of interventions that implement 2 components is less than the sum of BP reductions from interventions that implement each component alone.21, 57 Despite subadditivity, the BP effects of multicomponent interventions are often large and clinically relevant. One small but tightly controlled trial that enrolled hypertensive adults already on antihypertensive medication tested the effects of a comprehensive program of supervised exercise with provision of prepared meals to accomplish weight loss, sodium reduction, and the DASH diet. The program substantially lowered BP (net reductions in daytime ambulatory systolic and diastolic BPs of 12.1 and 6.6 mm Hg, respectively).110 A subsequent behavioral intervention trial, PREMIER, tested the effects of the major lifestyle recommendations (weight loss, sodium reduction, increased physical activity, and the DASH diet).111 In hypertensive participants, none of whom were on medication, mean systolic and diastolic BP reductions were 14.2 and 7.4 mm Hg (6.3 and 3.6 mm Hg, net of control). In nonhypertensive individuals, corresponding BP reductions were 9.2 and 5.8 mm Hg (3.1 and 2.0 mm Hg, net of control). Behavioral Interventions to Accomplish Lifestyle Modification A large number of behavioral intervention trials have tested the effects of dietary change on BP. A variety of theories and models have informed the design of these trials, including social cognitive theory,112 self-applied behavior modification techniques (behavioral self-management),113 the relapse prevention model,114 and the transtheoretical or stages-of-change model.115 Application of these models and theories often leads to a common intervention approach that emphasizes behavioral skills training, self-monitoring, self-regulation, and motivational interviewing.116 Typically, these trials enrolled motivated individuals, selected in part because of their self-reported readiness to change. Furthermore, these studies relied on skilled interventionists, often health educators or dietitians, who met frequently with participants. Characteristic findings of these trials are successful behavior change over the short term, typically 6 months, and then recidivism over the long term. The limited long-term success of intensive behavioral intervention programs highlights the importance of environmental changes that facilitate adoption of desirable lifestyle changes in broad populations. Indeed, even motivated individuals find it difficult to sustain behavior change given powerful cultural forces, societal norms, and commercial interests that encourage a sedentary lifestyle, a suboptimal diet, and overconsumption of calories. Despite these impediments, available evidence from efficacy studies is sufficiently robust and persuasive to advocate dietary change as a means to lower BP and thereby prevent BP-related cardiovascular disease in both nonhypertensive and hypertensive individuals. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Children Elevated BP begins well before adulthood, during the first 2 decades of life and perhaps even earlier, in utero.117 Numerous observational studies have documented that BP tracks with age from childhood into the adult years.118–120 Hence, efforts to reduce BP and to prevent the age-related rise in BP in childhood are prudent. The importance of these efforts is highlighted by evidence that BP levels and the prevalence of obesity in children and adolescents 8 to 17 years of age have increased between NHANES surveys conducted in 1988 to 1994 and 1999 to 2000.16. The effects of dietary factors on BP have been reviewed by Simons-Morton and Obarzanek.121 Unfortunately, most studies had methodological limitations, including small sample size, suboptimal BP measurements, and limited experimental contrast. At present, direct evidence from rigorous, well-controlled trials in children and adolescents is sparse. Accordingly, the effect of diet on BP in children and adolescents is, in large part, extrapolated from studies of adults. Such extrapolations are reasonable because elevated BP is a chronic condition resulting from the insidious rise in BP throughout childhood and adulthood. Older Persons Because of the age-related rise in BP that is particularly prominent in middle-aged and older persons and because of the high prevalence of BP-related cardiovascular disease, dietary strategies should be especially beneficial as adults age. Although most diet–BP trials were conducted in middle-aged persons, several were conducted in older persons.23, 122, 123 Other trials presented results stratified by age groups. Several important findings emerge. First, older persons can make and sustain dietary changes, specifically weight loss and dietary sodium reduction, over the long term.23, 24 Second, greater BP reductions from dietary interventions occur as individuals get older.29, 30 Third, because of high attributable risk associated with elevated BP in the elderly, the beneficial effects of dietary changes on BP should translate into substantial reductions in cardiovascular risk in the elderly.124. Blacks On average, blacks have higher BP4 and are at greater risk of BP-related complications6–8 than nonblacks. As documented previously in well-controlled efficacy studies, blacks as compared with nonblacks achieve greater BP reduction from several nonpharmacological therapies, specifically sodium reduction, increased potassium intake, and the DASH diet. The potential benefits of these dietary approaches are amplified because survey data indicate that blacks consume high levels of sodium while their potassium intake is less than that of nonblacks.43 In this setting, the potential benefits of dietary change are substantial and should provide a means to reduce racial disparities in BP and BP-related cardiovascular disease.125. Healthcare Providers Through advice and by example, physicians can have a powerful influence on their patients’ willingness to make dietary lifestyle changes.126 Although behavioral counseling is often beyond the scope of many office practices, simple assessments (eg, measurement of BMI) and provision of advice typically is feasible. The success of physician-directed and office-based attempts to achieve lifestyle changes is dependent on several factors, including the skills of the physician and staff, available resources, organizational structure of the office, and the availability of management algorithms that incorporate locally available resources. Individualized physician-directed lifestyle advice should be based on the patient’s willingness to adopt lifestyle changes. Motivated patients should be referred to a skilled dietitian, health educator, or behavioral change program, in large part because success will require frequent visits and contacts. Still, even without the assistance of ancillary personnel and programs, physicians should routinely encourage lifestyle modification. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A substantial body of evidence strongly supports the concept that multiple dietary factors affect BP. Dietary modifications that effectively lower BP are weight loss, reduced salt intake, increased potassium intake, moderation of alcohol consumption (among those who drink), and consumption of an overall healthy dietary pattern, called the DASH diet. Other dietary factors may also affect BP, but the effects are small and/or the evidence is uncertain. In view of the increasing levels of BP in children and adults and the continuing epidemic of BP-related cardiovascular disease, efforts to reduce BP in both nonhypertensive and hypertensive individuals are warranted. Such efforts will require individuals to change behavior and society to make substantial environmental changes. The current challenge to healthcare providers, researchers, government officials, and the general public is developing and implementing effective clinical and public health strategies that lead to sustained dietary changes among individuals and, more broadly, among populations. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||